This article originally appeared in the Winter 2021 issue of the Ontario Medical Review magazine.
Strong health-care system key to strong economy
Physicians and health-care partners have been speaking out for decades about the worrying state of health care in Ontario.
Unacceptable wait times for patients. Inadequate long-term care, home care and mental health and addiction programs. Inequities in the north and in low-income and racialized communities. Those problems, and many more, have been magnified by the COVID-19 pandemic, pushing the health-care system into an unprecedented crisis, with a staggering backlog of almost 20 million health-care services.
The pandemic has also proved that Ontario cannot have a strong and sustained economy without a robust, resilient and reliable health-care system that reduces the need for lockdowns and other measures in a public health emergency.
The OMA is sharing its recovery plan with the public, politicians, stakeholders and health-care system partners to reinforce what needs to be achieved to rectify years of neglect and underfunding of our health-care system.
“The urgent need to focus on solutions to improve patient care is a top priority for the profession. Physicians have a prescription for the future of health care and a roadmap to transformation for Ontario.” —Dr. Adam Kassam
The Ontario Medical Association, representing the province’s 43,000 doctors, has released a new plan to tackle these problems and transform the health-care system over the next four years.
“The urgent need to focus on solutions to improve patient care is a top priority for the profession,” OMA President Dr. Adam Kassam said. “Physicians have a prescription for the future of health care and a roadmap to transformation for Ontario.”
The OMA’s plan, Prescription for Ontario: Doctors’ 5-Point Plan for Better Health Care, is the result of the broadest consultation in the organization’s 140-year history. More than 110 health-care organizations, social service agencies and community leaders provided input. Almost 8,000 Ontarians from 600 communities shared their views last spring and summer through an online survey. More than 1,600 physicians representing a wide range of specialties and regions gave their expert advice.
Prescription for Ontario: Doctors’ 5-Point Plan for Better Health Care has 75 recommendations to strengthen the system and improve patient care provincewide in five priorities areas:
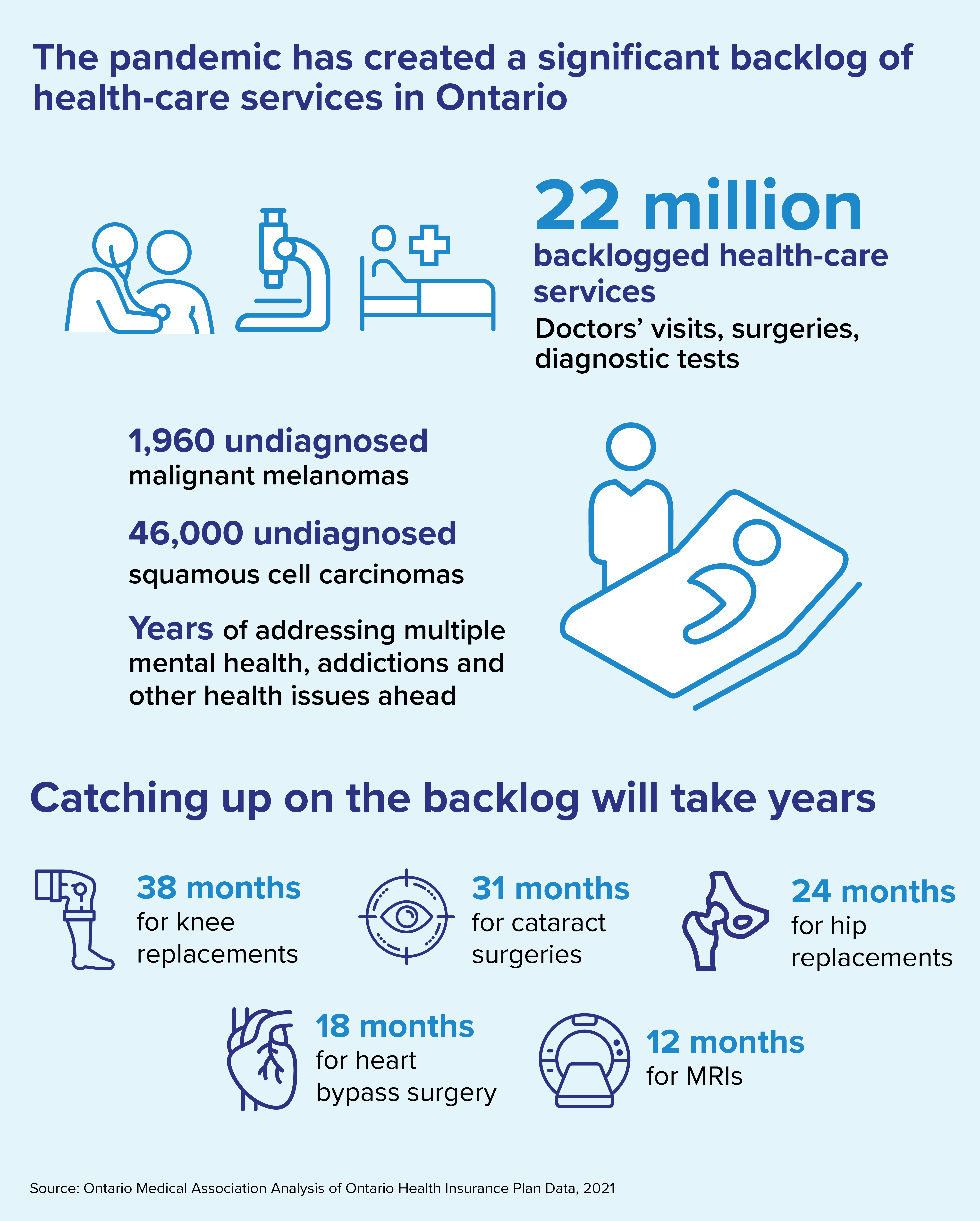
The most immediate crisis facing Ontario’s health-care system is the backlog of almost 20 million services, including visits to doctors, diagnostic tests, cancer screening, routine immunizations, treatments and surgeries.
Doctors are seeing patients sicker than they ought to be because of serious conditions left undetected or untreated during the pandemic. However, focusing on the pandemic backlog alone ignores the bigger problem — an inefficient health-care system with too few doctors, who are not linked digitally.
To clear the backlog of services and procedures, the OMA says doctors, nurses and other health-care workers would have to work considerably more hours than they already are over many months and years:
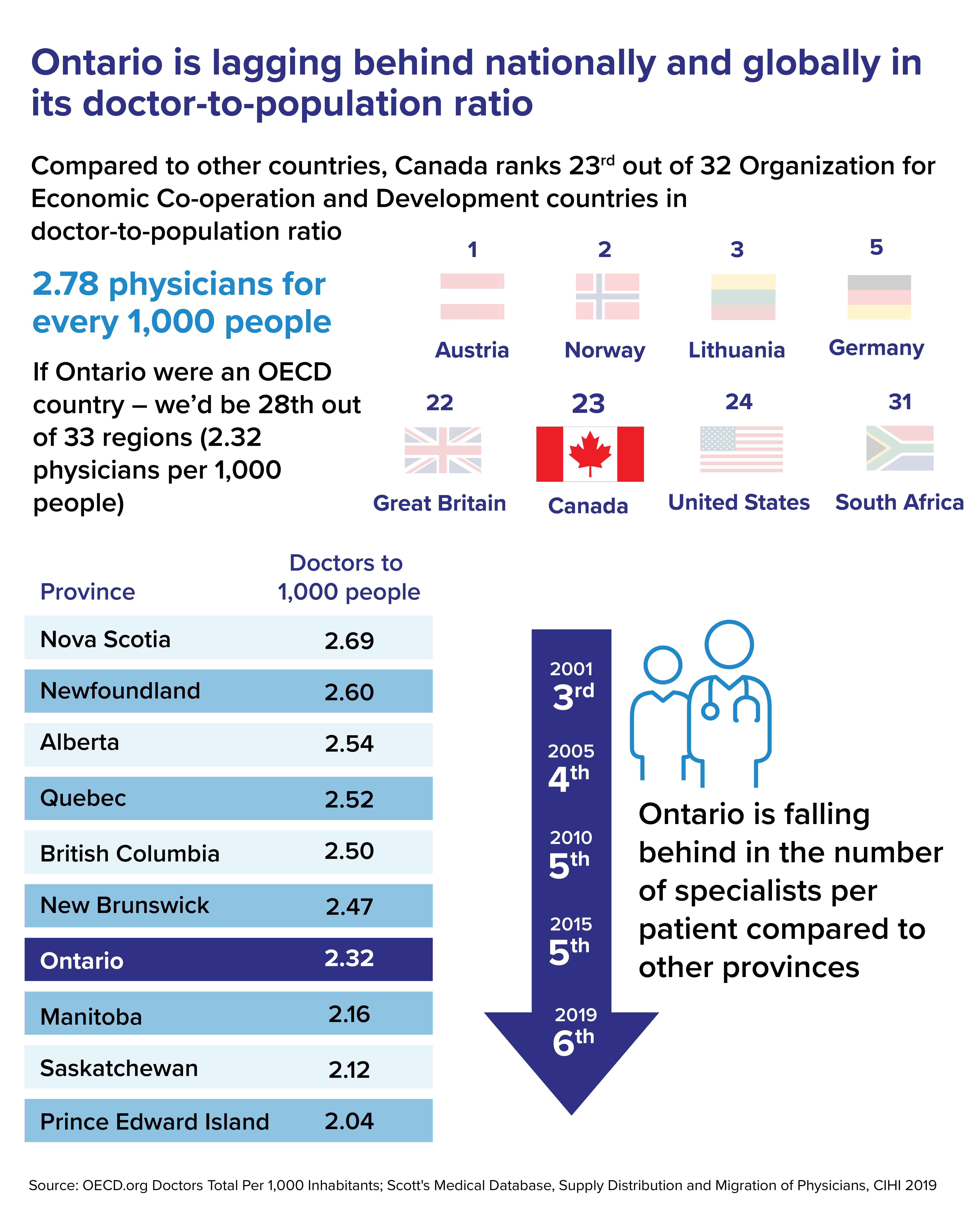
There are serious shortages of doctors and other health-care professionals in many regions, especially in the north and rural communities. One million Ontarians don’t have a family doctor. We know that access to care starts with the family doctor.
Ontario ranks seventh among Canadian provinces in number of family doctors per 1,000 patients (2.3) and has one of the lowest doctor-to-population rankings among OECD countries (28 out of 33). Prescription for Ontario: Doctors’ 5-Point Plan for Better Health Care also points out that many doctors are retiring or leaving the profession because of burnout exacerbated by the COVID pandemic.
Ontario spends less on health care per capita than any other province in Canada except British Columbia, according to data from the Canadian Institute for Health Information. This was due, in part, to a decrease in per capita spending in the 1990s, flat spending between 2012 and 2016 and spending below the minimum required to keep pace with demand in other years. Ontario’s per capita health-care spending is about eight per cent lower than the average of other provinces, according to CIHI.
The Ontario government can’t fix the ailing health-care system on its own, OMA CEO Allan O’Dette said.
“It requires collaboration among health providers, support from the public and political will. This requires significant investment from the federal government, including increased spending through the Canada Health Transfer to the provinces to cover 35 per cent of all health-care costs, up from the current 22 per cent,” O’Dette said.
And investing dollars in the health-care system is not enough, the OMA report said. Planning a better system must remove regional disparities and recognize that social determinants of health — income, education, food security, housing and early childhood development — are key factors in health outcomes, as is the need for action on climate change to mitigate its severe consequences on human health.