Vaccine hesitancy
The increasing number of Canadians who refuse or delay vaccination presents a challenge for physicians. This is especially concerning given the link between recent outbreaks of vaccine-preventable diseases (VPDs) and under-vaccinated communities.
Vaccine hesitancy is a complex behaviour that involves:
- Confidence (not trusting a vaccine or health-care provider)
- Complacency (not believing that vaccines are necessary)
- Convenience (ease of access)
Spectrum of vaccine hesitancy
Vaccine hesitant has replaced traditional phrases like pro- and anti-vaccine to better describe the broad spectrum of beliefs around vaccination, ranging from total acceptance to complete refusal.
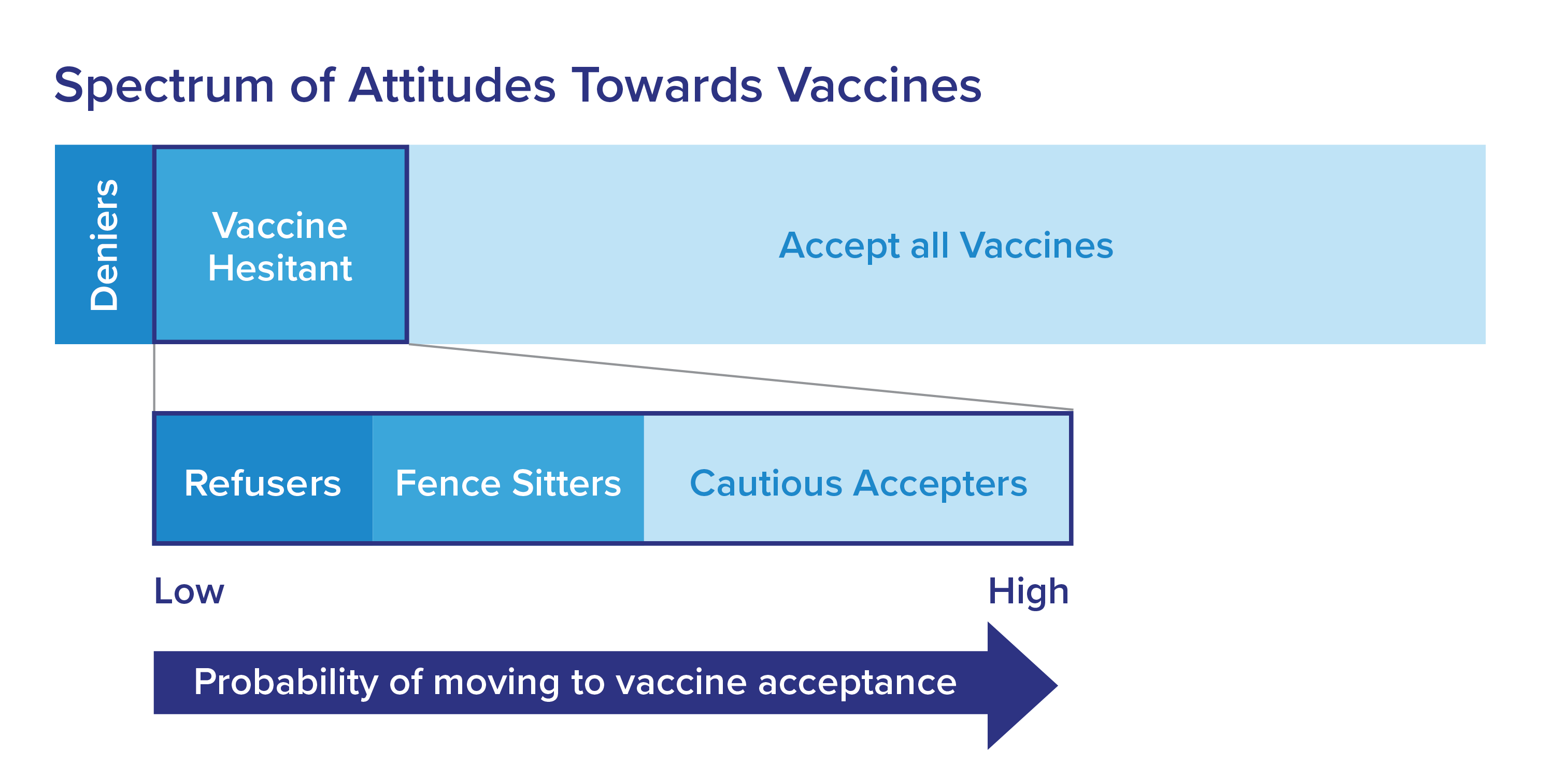
Vaccine-hesitant patients and parents are mostly fence-sitters and mild refusers who are a more attentive group with a greater chance of being persuaded to vaccinate. It’s more efficient to focus your efforts on these groups instead of firm refusers and deniers. An occasional brief check-in with deniers is enough.
Most undecided individuals respond well to vaccine information and many eventually consent after their concerns are heard and addressed. Nearly 80 per cent of parents report that the physician positively affects their decision to vaccinate their children.
If you find yourself in a situation where a patient refuses vaccination, it’s important to recognize the risk that unvaccinated patients may present to others while in your office. Take every possible precaution to minimize this risk and make sure you put in effort to understand your professional rights and responsibilities regarding vaccines.
More than 90 per cent of Canadian parents complete the full vaccination schedule for their children. Nineteen per cent of parents consider themselves to be vaccine-hesitant and about three per cent refuse all vaccines for their children.
Your role as a physician
As a physician, you are in a unique and powerful position to instill confidence in vaccine-hesitant patients and parents. Learn more about your responsibilities.
More than two-thirds of Canadian parents trust physicians as the most reliable source of information when it comes to vaccination. The effectiveness of your vaccination recommendations depends largely on how you communicate with your patients or their parents.
Physicians have the skills to build a relationship and correct vaccine hesitancy by:
- Demonstrating knowledge and compassion
- Using specific conversation approaches to positively influence people
These conversation approaches work well because they are based on understanding an individual’s perspective and core principles of shared decision-making.
Vaccine-hesitant groups
Vaccine-hesitant individuals fall into one of the following groups:
- Cautious accepters ultimately accept vaccines but may have minor concerns
- Fence-sitters accept some vaccines and delay or refuse others because they have a serious concern (for example, distrust in the health-care system, safety concerns, religious beliefs)
- Refusers might change their minds with increased trust and new knowledge
- Deniers reject all vaccination and react strongly to people who try and change their minds. They are hard to challenge and effectively impossible to sway
Strategies to improve vaccination rates
You can also help increase vaccination rates by:
- Improving access to vaccination by offering longer clinic hours or encouraging patients and parents to receive vaccines, where permitted by law, through other health-care providers such as pharmacists
- Increasing vaccination demand by sending out reminders to patients and parents. For example, letters, phone calls and text messages
- Providing passive education to patients and parents. For example, posters, booklets and videos on VPDs and vaccination in waiting areas and offices. Refer to curated resources and practice tools