About fee-for-service post-payment reviews
The Plan to Build Ontario Together Act included amendments to the Health Insurance Act (HIA) to make OHIP more accountable, which included the introduction of a new physician payment review process in Ontario that is intended to be fair and impartial, accountable and transparent.
After the initial tabling of the bill, the OMA expressed serious concerns with many proposed provisions in Schedule 15, and the Minister of Health pledged to work with the OMA to find a fair and equitable solution. The OMA and ministry entered into discussions and subsequently agreed to a series of amendments to Schedule 15 that removed many of the provisions that were most problematic for physicians, clarified the government’s intention, and revised the audit process to ensure that it contains necessary procedural safeguards, while maintaining the overall objective of accountability and transparency, with a focus on education. In December 2019, the government introduced amendments to Schedule 15 of the bill, which subsequently passed.
When the OMA and ministry discussed revisions to Bill 138, the ministry committed to working with the OMA in the development of policies and procedures with respect to post-payment accountability, including implementation. The objective was to implement the process, balancing the government’s responsibilities with respect to payment accountability and fairness to physicians within the framework of the amended HIA. The OMA and the Ministry of Health jointly developed the following documents, which reflect a clear, balanced and objective tone, while reinforcing the principles of transparency and fairness, and promoting physician confidence in the new system.
Summary of the physician fee-for-service post-payment audit process
The Ministry of Health (the “ministry”) has committed to providing information to assist physicians with appropriate claims submissions in order to receive the payment they are entitled to for the provision of Ontario Health Insurance Plan (OHIP) insured services. The ministry and the Ontario Medical Association (OMA) provide billing education and other supports to assist physicians with questions and with understanding the appropriate fee codes to submit for the services provided.
OHIP payment requirements are set out in the Health Insurance Act (HIA) and Regulation 552 (including the Schedule of Benefits for Physician Services). Learn more about these acts and regulations.
The ministry’s post-payment review process is governed by various principles designed to ensure procedural fairness, integrity, transparency and accountability, as required by law, including:
- Impartiality in the selection of physicians for review
- Staff who are trained in the process of post-payment audit
- The ability to dispute a general manager’s opinion at the Health Services Appeal and Review Board (HSARB), meaning that unless there is a voluntary settlement between the physician and the GM, payments can only be Recovered following an order of that tribunal
- The GM of OHIP to demonstrate at HSARB that an order should be made
- The ability to retain legal representation at any time in the process
- Privacy and confidentiality maintained throughout the audit process
- An emphasis on professional and courteous behaviour
- Timely communication of all relevant information
- The ability to provide information to the GM throughout the audit process
- The ability to make written or oral submissions at the HSARB
- The ability to submit a complaint about ministry conduct during audits without fear of reprisal
For ease of reference and to help understand some of the commonly used terminology, read the glossary of terms.
To facilitate payment of the high volume of claims submitted, claims are paid on an honour system after being processed through automatic computerized checks, which apply payment requirements in accordance with the HIA, Regulation 552 and the Schedule of Benefits. As not all payment rules can be computerized, these initial checks and the resulting payment do not necessarily mean that all payment requirements have been met.
Under the authority of Section 18 of the HIA, post-payment reviews of physicians’ claims for payment may be performed as a component of measures that contribute to overall accountability for the use of OHIP funds and ensures that payments made by OHIP are authorized by the HIA. Section 18 and Schedule 1 to the HIA describe the ministry’s authorities and the process for post-payment review of physician payments (read section 18 and Schedule 1 of the HIA). For example, subsection 18(8) of the HIA allows the ministry to refer a post-payment billing review matter to the Health Services Appeal and Review Board if the general manager of OHIP forms the opinion that one of the following circumstances exists:
- All or part of the insured service was not in fact rendered
- The service was not rendered in accordance with the HIA and the regulations Thereto
- There is an absence of a record, as described in section 17.4 of the HIA
- The nature of the service is misrepresented, whether deliberately or inadvertently
- All or part of the service was not medically necessary (after consulting with a physician)
- All or part of the service was not provided in accordance with accepted professional standards and practice
The ministry conducts post-payment reviews of physicians’ OHIP claims in accordance with applicable law and policy. The purpose of these reviews is to identify potential billing concerns, to communicate with physicians and to provide billing education to ensure that future claims for payments meet the requirements of the HIA.
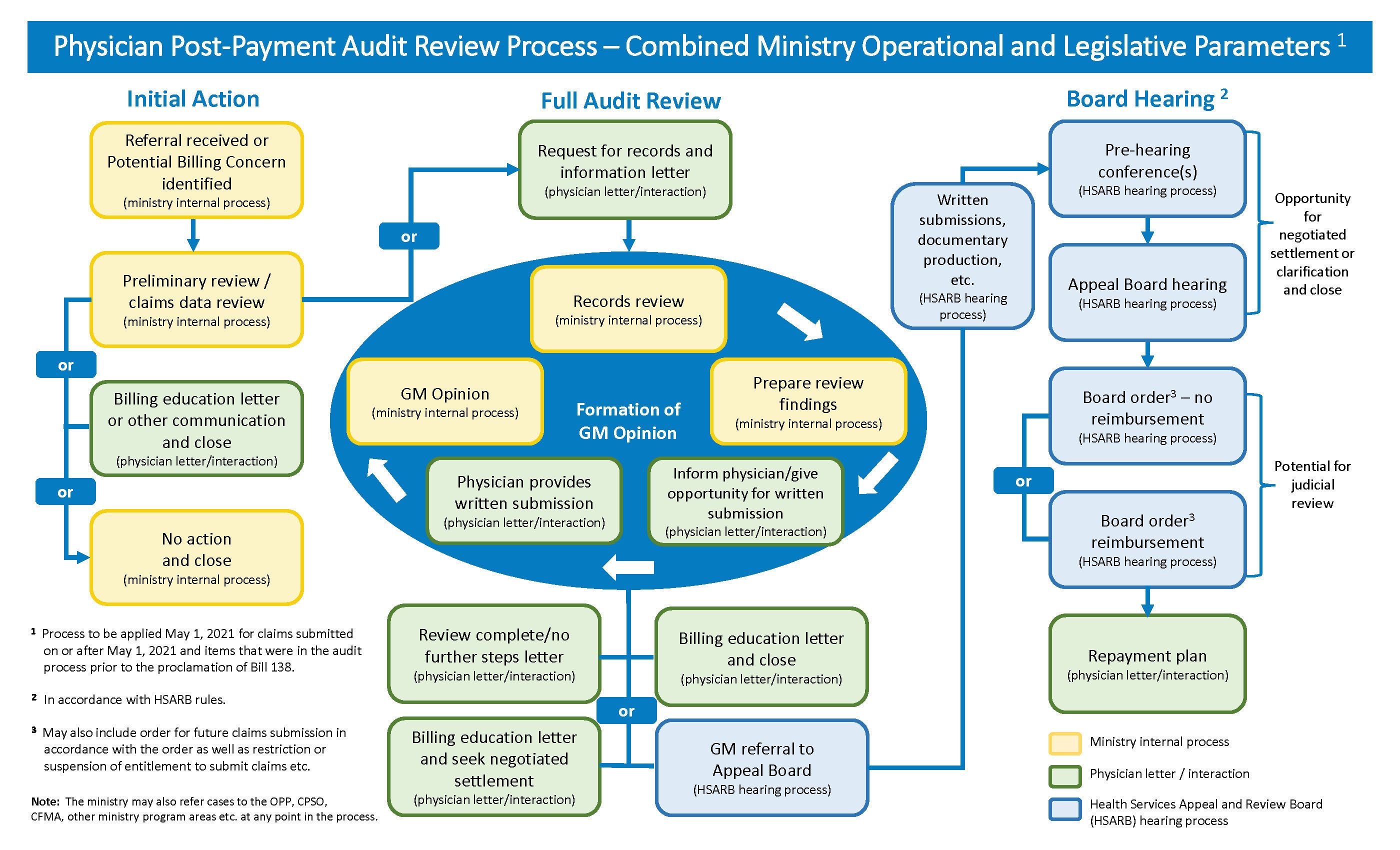
The three main stages of a post-payment review are initial action, full audit review and board hearing.
Not all reviews progress through all stages of the process. Negotiation of a settlement can happen at any point in the process. Learn more about the stages of a post-payment review or download the physician post-payment process review diagram.
This explanation of the ministry’s general process for audit of physician payments is provided so physicians are aware of what to expect if their claims are reviewed and understand the general factors the ministry considers in the post-payment review process. This explanation does not replace the law and processes set out in the HIA. It is important to recognize that all reviews are guided by the factual nature of the audit and that review steps are determined on a case-by-case basis, with consistent and impartial application of the audit process and payment requirements.
Physicians are entitled to seek legal advice and to be represented by legal counsel during this process.
In performing post-payment audit reviews, the ministry is committed to educating physicians on appropriate billing. In addition, the ministry will treat physicians professionally, courteously and with respect throughout the process, provide procedural fairness, ensure privacy and confidentiality, and pay providers for the insured services they deliver to patients as required by law. The ministry does not release audit information to the public unless required by law to do so.
Contact us
Members are encouraged to reach out to the OMA if they require further information or clarification, and to contact the CMPA if they require representation and assistance in responding to a post-payment audit.