This article originally appeared in the September/October 2020 issue of the Ontario Medical Review magazine.
OMA webinar explores the importance of meaningful physician engagement in health system transformation
By Stuart Foxman
For the sake of patient well-being and physician leadership, it’s the most significant opportunity in decades. That’s how Dr. James Wright, Chief, OMA Economics, Policy & Research, characterized Ontario Health Teams (OHTs).
Dr. Wright was speaking this September at an OMA virtual session on meaningful physician engagement and governance. He said that OHTs are a chance to fundamentally change the system and integrate care.
At the outset of the conference, Dr. Adam Kassam, the OMA’s President-Elect, welcomed a redesign that brings together a network of doctors with “a unified voice.”
Under OHTs, health care providers work as one co-ordinated team, no matter where they are. The first OHT cohort was announced in late 2019. There are now 29 across Ontario, with 17 teams invited to move on to the next phase of the readiness assessment process and complete full applications.
The ultimate goals are to deliver high-quality care, connect patients to the different types of services they need, and provide 24/7 help in navigating the health system. (See sidebar.) How can we get there?
For insight into why and how groups like OHTs can be effective, the session heard from an outside voice: keynote speaker Dr. Paul Harkaway. He’s a pulmonologist and critical care specialist in Michigan with extensive experience with ACOs – accountable care organizations.
An ACO is a network of doctors and hospitals that shares financial and medical responsibility for providing care. Dr. Harkaway said the objective should be no needless pain or suffering, no needless deaths, no helplessness in those served, no unwanted waiting, and no waste, for anyone, ever.
How do you do it? You build a “thing”, he said. It’s not a building, a staff committee, a new medical speciality, a drug or a device. It’s not a financing organization. Instead, it’s a care organization, revolving around patients.
This “thing” will have memory of patients, not amnesia, he said. It will attend to handoffs, manage resources, and reduce dependence on the hospital. All while proactively tracking outcomes and continuously improving.
Why participate in a model that can involve additional work and energy? Simple, said Dr. Harkaway: the system currently delivers poor quality. That’s not the intent and isn’t a critique of the capabilities of individual doctors. But as a system, he said, the quality of care and the experience is too low, costs are too high, and the waste is excessive.
Doctors can’t serve patients well in a dysfunctional system. Dr. Harkaway, however, put the challenge to doctors and the potential repercussions bluntly. Doctors as a professional responsibility need to do their part in changing the system, and holding themselves accountable.
“We have to be more than kind, caring doctors taking care of patients one at a time,” he said.
The quadruple aims are better patient and population health outcomes; better patient, family and caregiver experience; better provider experience (Dr. Harkaway talked about returning joy to the practice of medicine); and better value. To all that, you could add a fifth aim: greater equity.
Why must physicians lead entities like ACOs and OHTs?
Dr. Harkaway pointed to four reasons:
Doing that, Dr. Harkaway said, requires “a comprehensive, committed, courageous, community of clinicians building consensus.” Know the patient in the deepest sense, keep them out of hospitals or nursing homes if possible, and focus on sick care first, not on the social determinants of health. While those determinants are critical, he said doctors ultimately should focus on what’s directly under their control.
Where are we on the OHT journey? Dr. Wright followed Dr. Harkaway by discussing the value equation, and why doctors should sign on to this “somewhat aspirational” idea.
For one, physicians, patients and the OMA have long advocated for integrated care. The OHT vision is that physicians will spend less time co-ordinating care, and more on what they do best – caring for patients.
Dr. Wright emphasized three principals that OMA has talked about: OHTs should be voluntary, physician-led (in terms of governance), and primary care-based (though not to the exclusion of specialists). He said evidence shows that physician leadership is critical in improving the quality of patient care in OHTs (and is more likely to engage other physicians).
Doctors have some legitimate concerns. Will the government compel any doctors to participate in OHTs? No, stated Dr. Wright. Will doctors become employees of OHTs? No. Will they be compensated for non-clinical OHT work? They’ll have to, or OHTs won’t be sustainable. How will physicians lead OHTs and be heard? This needs to be grassroots. Will a future government abolish OHTs? They might call them something different, said Dr. Wright, but the movement to integration will not be stopped.
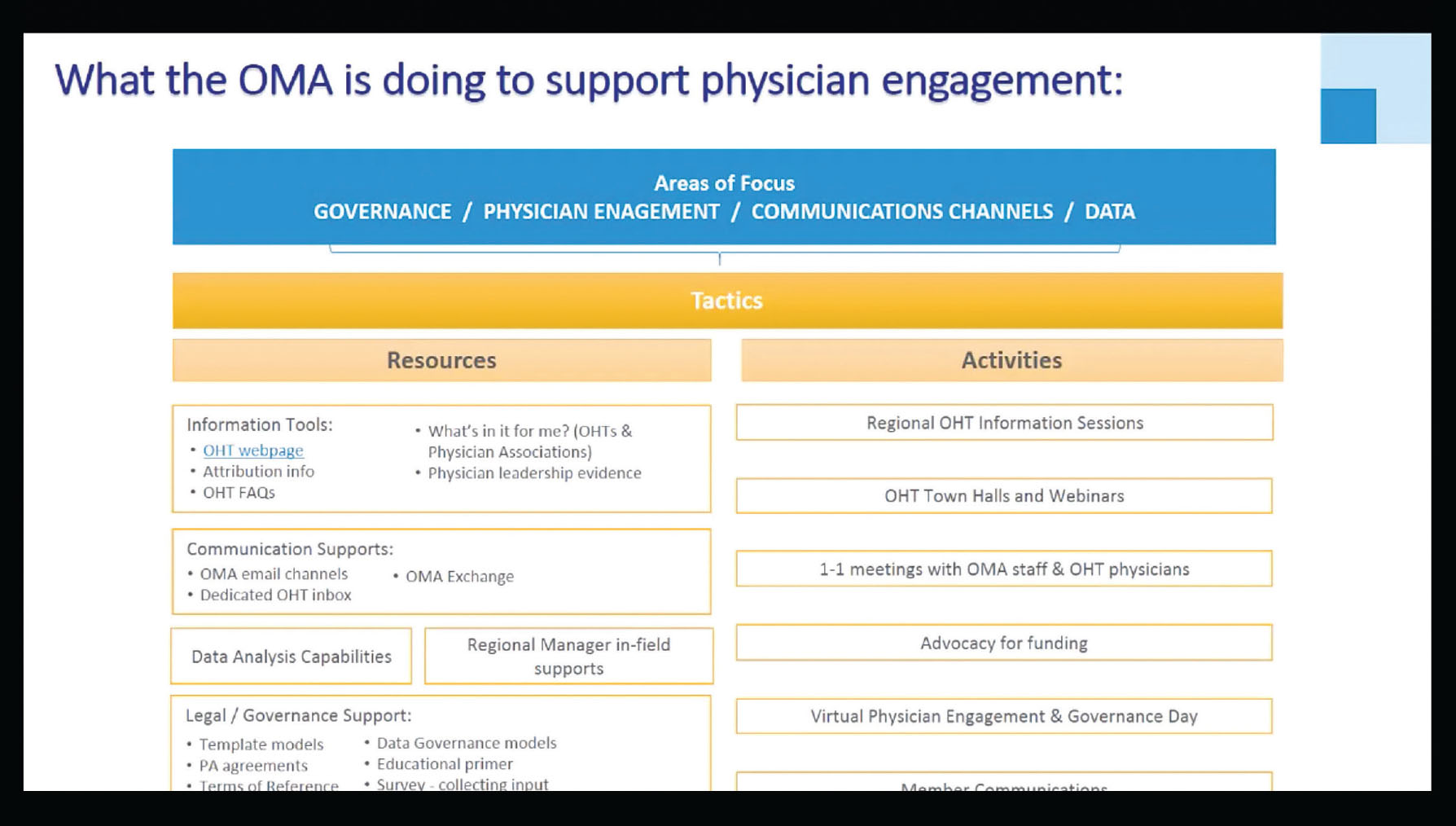
The OMA has encouraged physician leadership/engagement through an OHT webpage of resources, and presentations at many regional information sessions, town halls, and webinars. An OMA white paper shares early learnings from OHTs and recommendations for their evolution.
Dr. Wright referred to a recent survey of physician leaders from OHTs, showing that the number of physicians engaged and leading OHTs remains too low. There’s also relatively modest engagement with community-based specialists. A majority of respondents cited the lack of compensation for non-clinical work as a major barrier. Burnout remains another barrier.
Having said that, we’ve seen through COVID, for example, how well-organized physician networks can come together, respond to local issues and be impactful. While we need to do more to help doctors understand OHTs, Dr. Wright is confident that their time has come.
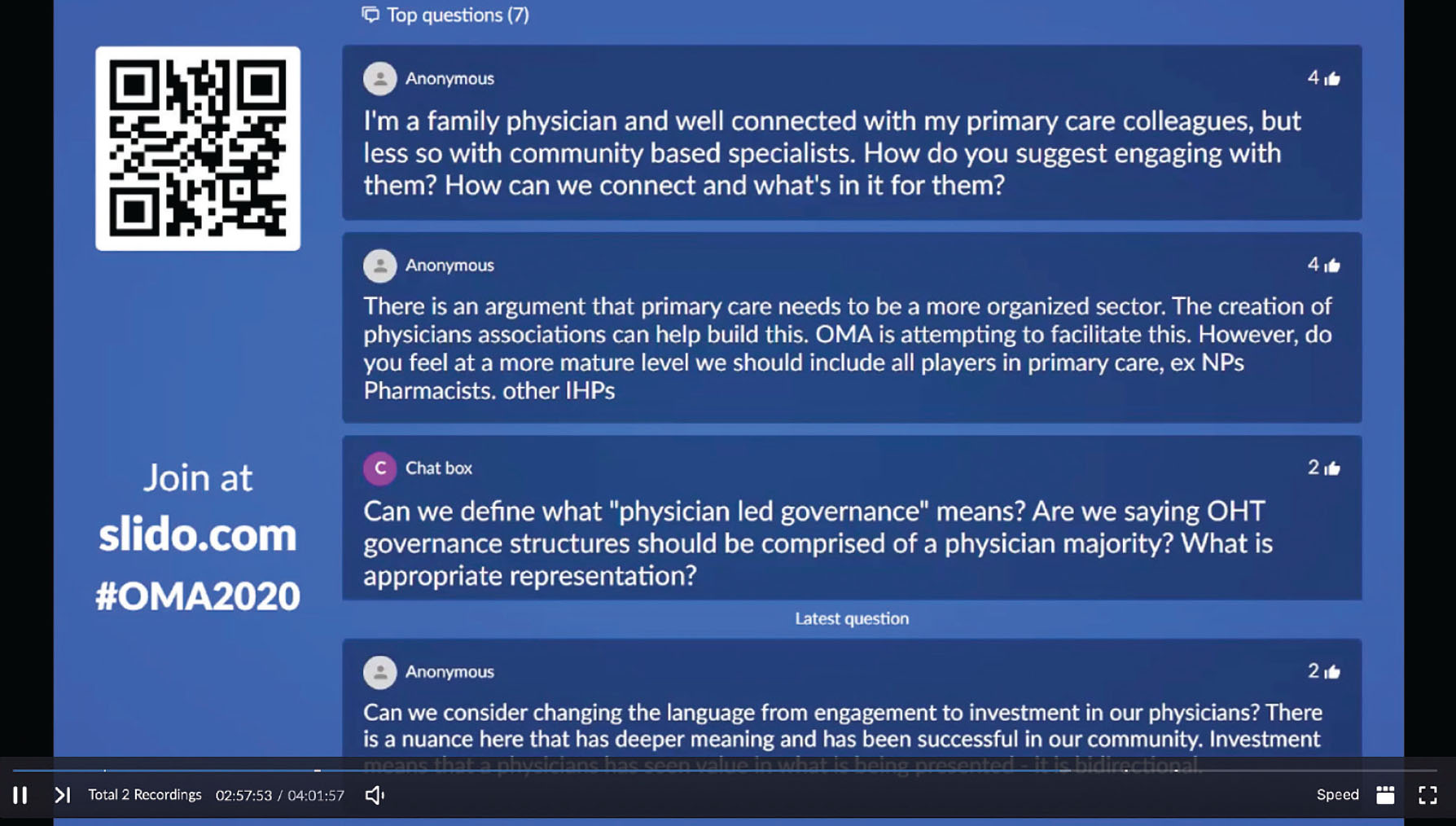
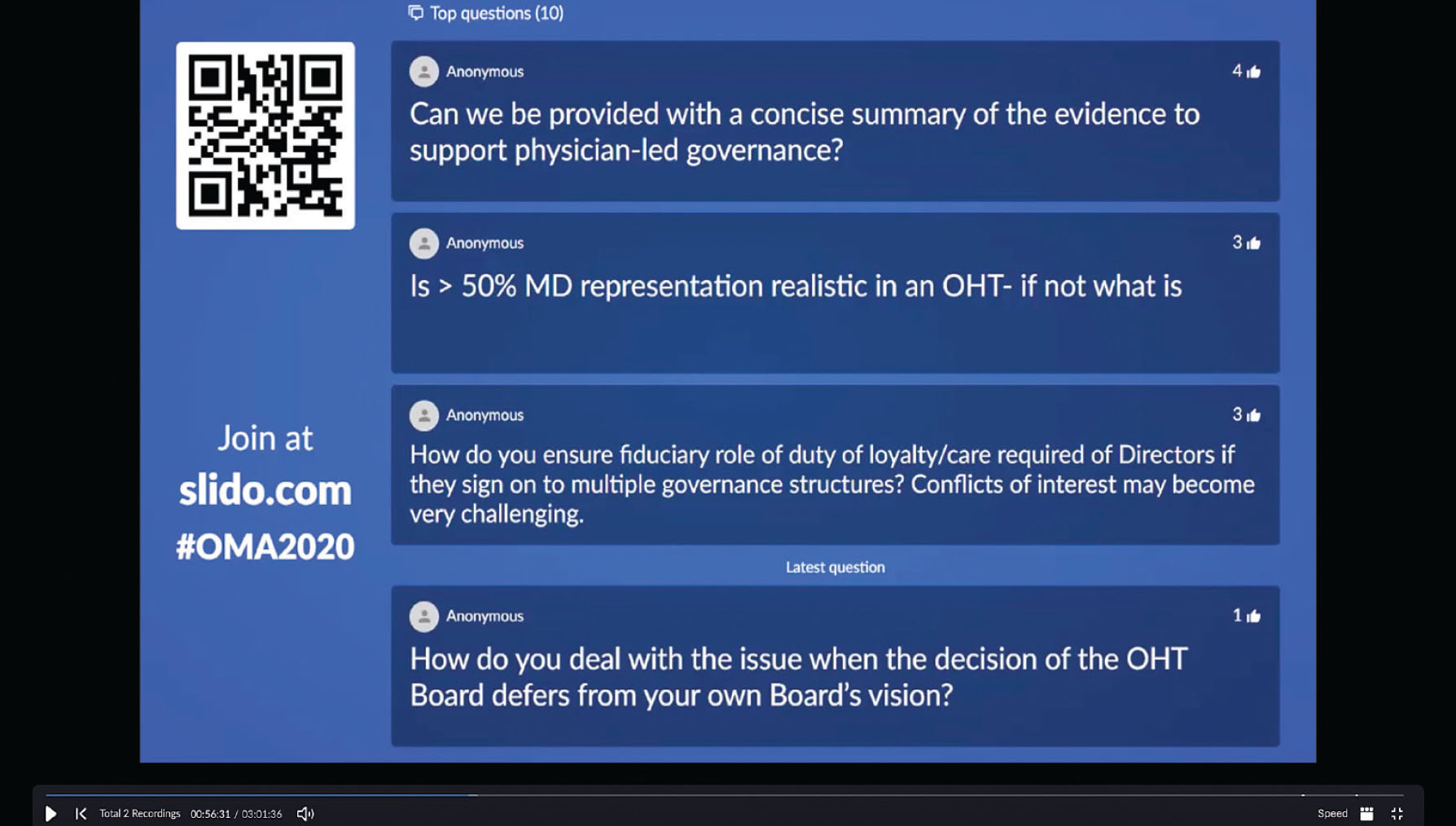
To discuss physician governance, the session heard from Jennifer Gold, OMA Director of Legal and Privacy. The Ministry of Health has not prescribed a specific governance structure for OHTs, so groups must develop their own.
Beyond that structure, OHTs may require new legal contracts, including an agreement or bylaws to govern the group members, and an overarching agreement between the OHT and the Ministry of Health/Ontario Health. Members of an OHT may also need or want additional agreements to define accountability and funding relationships, or to explain how care will be provided or co-ordinated. The OMA can offer guidance based on expertise in this area.
Most OHTs have not yet formalized their governance structure, which is good, said Gold. This will be a work-in-progress, and models will evolve. The primary objective should be to ensure that physicians have a major voice at the table.
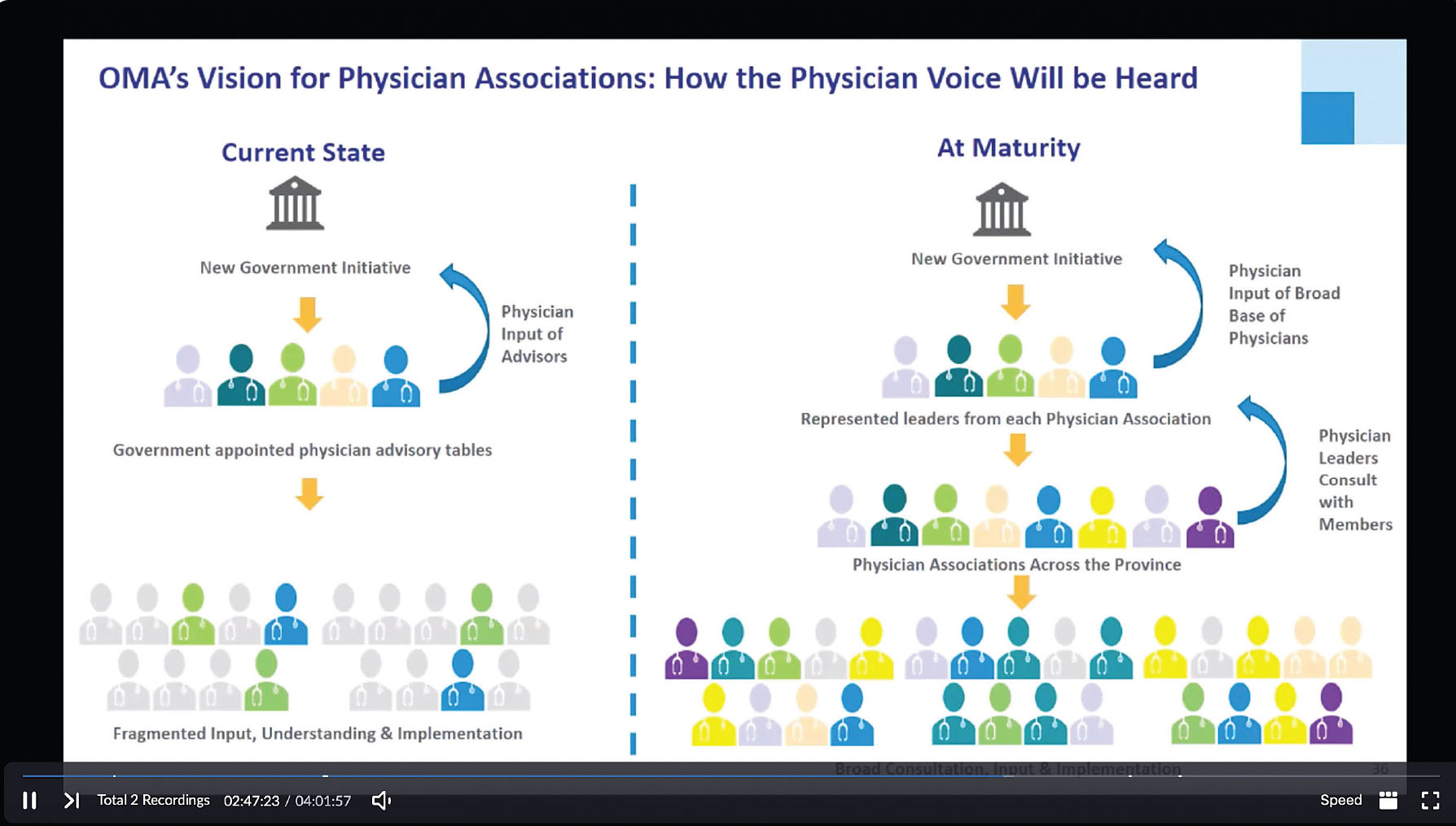
Gold said most physician leaders working on OHTs are self-identified, therefore have no real representative authority to speak on behalf of the group. At this early stage, she recommends physician groups organize into an unincorporated association, as these are more easily modified than formal corporate structures.
Among the governance issues to address: who will be elected, when and how often do they meet, how do they make decisions or resolve disputes, and what happens when people leave.
Gold said there’s no risk to signing on to a physician association. You can withdraw any time. The benefit is a chance to lead the way. “If physicians don’t lead, someone else will step into that vacuum,” she said.
A panel discussion explored some ways to help doctors see the appeal of OHTs. It’s powerful to have a network of “activated primary care leaders”, said Dr. Rob Annis, a general practitioner in Listowel, and physician leader at the Huron Perth OHT.
He told participants that you need solid relationships with community care providers, and should focus on solutions to local problems rather than on the OHT structure. This is an opportunity to level the playing field in team-based care, said Dr. Annis, who is Past President of the Association of Family Health Teams Ontario, and former Chief of Staff of the Listowel Memorial Hospital.
Some worry that hospitals will take over OHTs. Dr. Paul Woods, President and CEO of London Health Sciences Centre, and a family physician himself, offered reassurances. He understands the need for physician-led OHTs, and invites them to make the compelling case for how this will help to solve some of the problems that hospitals are facing. That would be persuasive.
What else can get physicians to participate? The clear potential to meaningfully contribute to actual change.
“It’s about providing the evidence,” said Dr. Rebecca Stoller, a family physician in the North York Toronto Health Partners (NYTHP) Ontario Health Team.
The panel was asked whether every OHT should evolve in a slightly different direction, or should we land on one provincewide initiative?
The more things are unified, the easier they are to build, said Dr. Harkaway, but he advocated a mix of both approaches. Dr. Annis said some things must be done centrally, like data management solutions, but added that we have had years and years of top-down solutions. “We need to build from the ground up,” he said.
Dr. Woods called for a broader measurement system, with performance targets based on the local population. Be the change you want to see, he said. If we can do something that makes life better for patients, and takes costs out of the system, that’s powerful.
Deliver those results, said Dr. Woods, and most physicians will want to be part of it.
Stuart Foxman is a Toronto-based writer.