This article originally appeared in the September/October 2020 issue of the Ontario Medical Review magazine.
OMA-commissioned study identifies range of patient and caregiver preferences in how health care could be shaped or reshaped
The Ontario Medical Association continues to provide influential thought leadership in the area of health system transformation and renewal through the OMAThoughts reports. In late 2019, the OMA engaged the North American Observatory on Health Systems and Policies to conduct a scoping review of the literature in order to gain insight into the nuances of patient and caregiver preferences or desires across a variety of health and life stages. Highlights from the report, entitled Patients’ Views of the Canadian Health Care System, are provided below.
Patient-centred care is currently a priority area of inquiry among researchers, decision-makers, and health system planners. The COVID-19 pandemic has reinforced the importance of ensuring health and social care services are delivered to users in a meaningful and effective manner that meets their needs and preferences.
In order for patient-centred care to be meaningfully implemented, we first need to understand the needs, preferences and desires of a wide spectrum of patient groups.
Current patient engagement efforts tend to rely on subsets of patient perspectives, limiting our capacity to understand the full range of preferences needed to move toward patient-centred care. Additionally, we still have limited insight into how patient perspectives on health care can be used to inform system reform.
In 2019, the Ontario Medical Association’s Economics, Policy and Research (EPR) Department commissioned the North American Observatory on Health Care Systems and Policies to produce a study that provides insight into the health care experiences of patients and caregivers across multiple health and life stages.
Based on a literature review of 193 peer-reviewed articles, the NAO study categorized patients into two groups – health stage and life stage – to help identify and understand the differences and similarities that could inform health-system improvements. Results of the NAO study form the basis of the white paper, Patients’ Views on the Health Care System, released in September.
While this study was conducted prior to the COVID-19 crisis, the impact of the pandemic aligns with and confirms a number of its findings. For example, COVID-19 highlighted how different populations required different management, making it important to understand the attributes and needs of various groups of people. COVID-19 infections were higher among those in low socio-economic groups, racial minorities, the vulnerably housed and the elderly, especially those in long-term care homes. The white paper found that patients experienced biases in the health care system and want care that is free of racism, language barriers and discrimination toward religions, cultures, gender identities and socioeconomic status.
This study reveals similarities in desires across all patient health and life stages, which can be categorized into five broad themes: a desire for personalized care; a desire for information on resources available and how to navigate the health system; a desire for choice in treatment, care setting and/or care provider; a desire for holistic care and non-medical supports; and a desire for care co-ordination and care continuity.
However, even with these similarities across health stages, the way these preferences and needs were expressed, and the examples of changes to health care systems that were suggested, differed across patient groups.
These findings are novel as they highlight nuances in preferences and desires that are both similar and different across health stages. Findings from this study are timely as jurisdictions internationally aim to deliver patient/caregiver-focused models of integrated health service delivery.
Many of the desires echo features of successful integrated patient-centred care models. At the forefront of integrated care models are the real-life needs of patients and caregivers. Health systems across many provinces/territories in Canada are at the cusp of change, with integrated care at the forefront of the health policy agenda.
In Ontario, for example, we are seeing efforts toward integrated care, through the development of Ontario Health Teams which intend to bridge the gap between various sectors of the health system including home care. Improving care navigation by linking patients discharged from hospitals to community service groups, engaging patients and caregivers in health system design, improving access to virtual care options for patients, and connecting teams of providers and services to patients and families in the community is desired by patients and health systems.
Certainly, findings from this review are timely as provinces like Ontario continue to make strides toward a more integrated, patient/caregiver-focused model of health service delivery. Thus, these findings will be particularly helpful to inform the following efforts:
Through understanding the detailed experiences and preferences of a variety of target populations. This may inform which providers to consider being a part of the integrated care team.
In offering insight into the diversity of patient views across population groups and informing patient engagement efforts.
In informing the development of metrics that reflect the desires and preferences of patients and caregivers.
In identifying areas for investment that are relevant to, and important for, a variety of target populations.
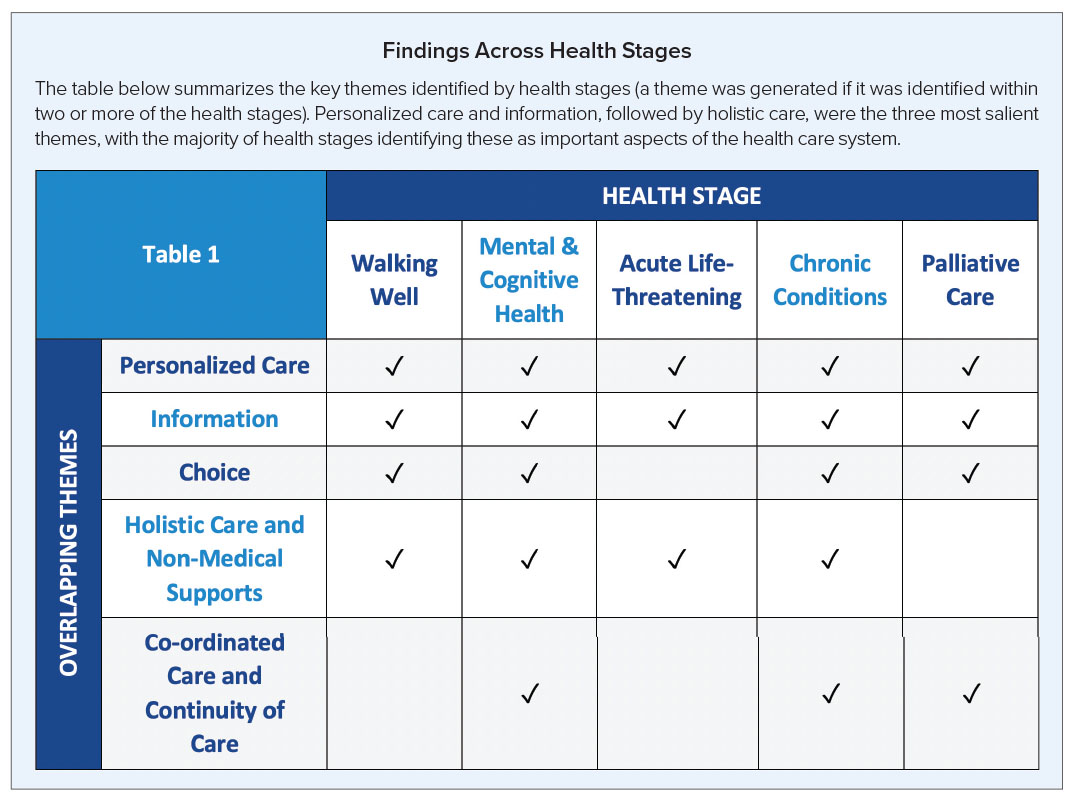
The table below summarizes the key themes identified by health stages (a theme was generated if it was identified within two or more of the health stages). Personalized care and information, followed by holistic care, were the three most salient themes, with the majority of health stages identifying these as important aspects of the health care system.
The NAO would like to acknowledge the instrumental support of the following people in conceptualizing this research study and for providing invaluable feedback at all stages of the project:
Dr. James Wright, chief, OMA Economics, Policy & Research; Dara Laxer, executive director, OMA Health Policy and Promotion; and OMA past president Dr. Nadia Alam. We also thank Dr. Kerry Kuluski for her extremely thoughtful feedback and expert review of this work.