This article originally appeared in the November/December 2020 issue of the Ontario Medical Review magazine.
COVID-19 year in review
by Stuart Foxman
Viruses don’t know calendars. As we turn the page from 2020 to 2021, COVID-19 is not behind us. While we’ve made progress, many hurdles remain. But the end of the year is a time to reflect on how the OMA has responded to the pandemic.
That started before the first case of COVID-19 was even confirmed in Ontario. The Economics, Policy & Research (EPR) team recognized the threat of COVID-19 early, and initiated the OMA’s response the week of Jan. 20, 2020. The OMA created a COVID-19 Action Group of more than 60 staff from key functional areas.
In this most challenging of years, how has the OMA provided support to members? Advocated for them? Offered timely advice to policy-makers? Communicated with the public? What are some of its biggest successes, and most important lessons?
One more question: Where do we go from here? It depends on how everyone does their part. Late in the year, as cases were again rising, OMA President Dr. Samantha Hill noted that everyone – including doctors working on the frontlines – is suffering from pandemic fatigue. We all yearn to return, as she said, to “the way things used to be.”
We are not there yet. However, a new year does bring the promise of a vaccine. There are reasons to be optimistic, especially if we continue to look after each other to get COVID-19 under control. “We are all in this together,” says OMA CEO Allan O’Dette, “and together we will conquer this.”
With COVID-19, circumstances evolve quickly. The OMA has been just as fast to respond to members’ information needs. To offer the latest news and guidance, the OMA worked with the Ministry of Health, the Chief Medical Officer of Health and health system partners. A dedicated section on the OMA website provides daily situation reports, notes on events and webinars, and quick links to data and other resources.
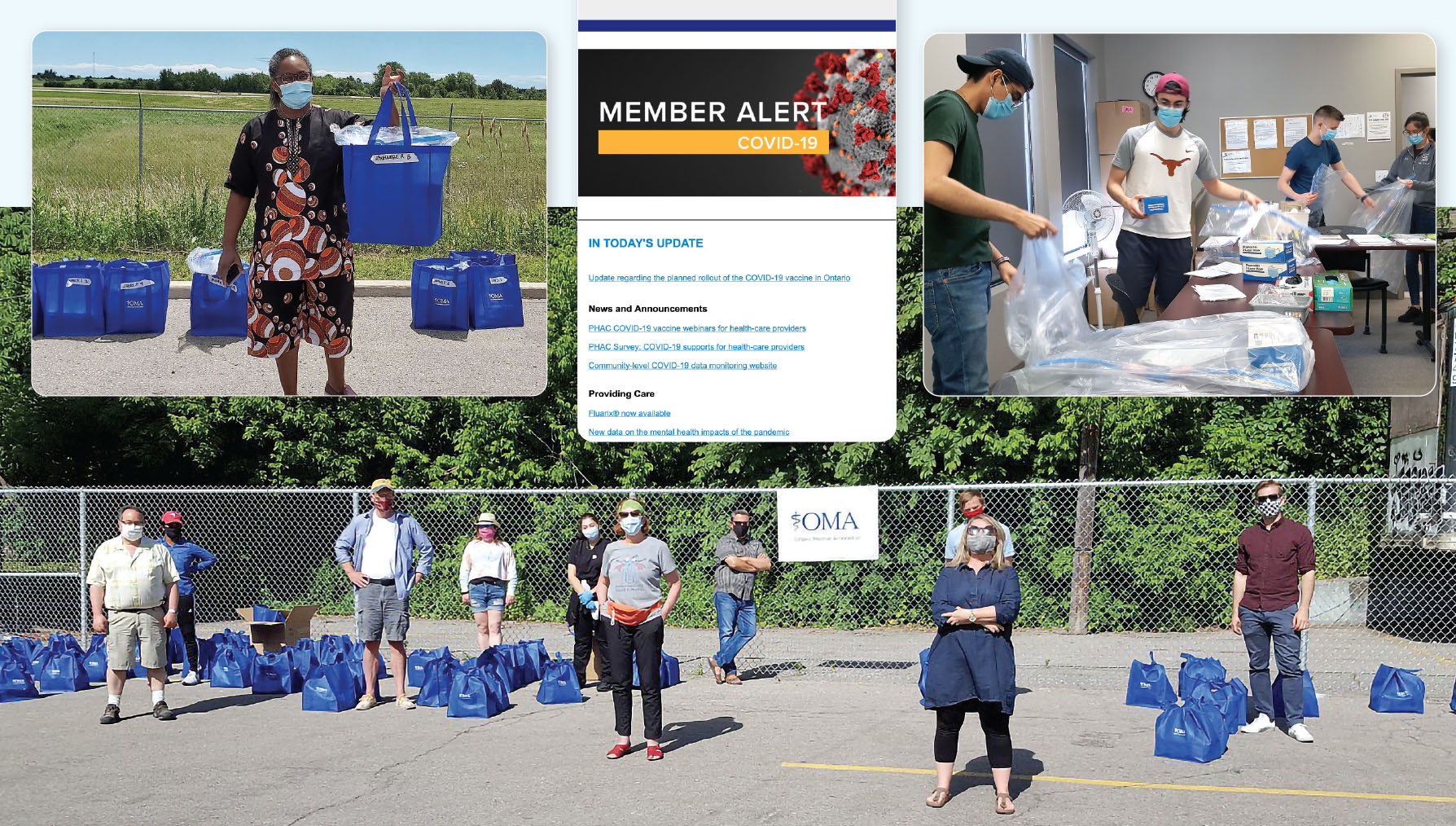
That includes the OMA Member Alert COVID-19 eNewsletter (published 77-plus times through to early December), covering everything from COVID-19 case maps, to patient-assessment tools, to checklists for in-person care. The OMA President’s Updates are another constant source of information.
COVID-19 has had major impacts on practices of all types. Helping members adjust, the OMA provided guides, flowcharts and FAQs around things like business continuity planning and human resources decisions. The OMA also supported members by holding several town halls, and responding to thousands of inquiries.
“Our members are going through a difficult time. It’s important that their Association is a reassuring voice,” says John Bozzo, Chief, Member Relations, Advocacy & Communications.
To help raise awareness around COVID-19 safety practices and protocols, the OMA developed several patient-focused tools and resources. They include Community Info Bulletins, a Contact Tracing Pocket Journal and a Personal Activity Log (for patients to track their contacts and symptoms). Physicians could download these tools to post in their medical offices and on practice websites, and to share online with patients.
Together, this information has helped members to stay atop a fluid situation, and best serve their patients.
COVID-19 has placed a premium on sound and clear advice. “In any crisis, you need to be credible, relevant and timely in communications,” says Bozzo. The OMA filled the need by:
The public looks to doctors and the OMA as trusted sources of information. Keeping Ontarians informed was an important part of keeping them safe, too.

When a crisis hits, resources of all sorts can be in short supply. The OMA worked hard to get doctors what they needed most. At a basic supply level that included ensuring sufficient personal protective equipment (PPE) for community-based practices and long-term care homes. The OMA supported multiple PPE drives via social media and media relations, led a public campaign to underscore the need for frontline staff, and developed a list of preferred PPE vendors.
While many Ontario physicians were fighting hard against COVID-19, others were hard hit. They faced delayed payments and financial challenges, and some offices and clinics risked closing. The OMA advocated for more appropriate government funding, and for virtual care OHIP codes. Shifting gears, the OMA paused the 2021 Negotiations Task Force (NTF) and transitioned to the COVID-19-NTF. Regarding compensation for hospital-based physicians, the OMA provided strategic advice and support to the NTF during negotiations with the government.
From October 1, 2020 until March 31, 2021, the Ministry of Health has agreed to reinstate funding for infectious disease hospital-based specialists and physicians performing temporary non-clinical assignments. That’s welcome, but isn’t nearly enough. The OMA continues to push for additional measures to respond to the second wave of COVID-19. In these and other efforts, the broader goal is to ensure the well-being of the public and the health care system. All so that the health care infrastructure can remain strong through the pandemic, and beyond.
To ensure they could meet surge demands, health care facilities needed a ready supply of doctors. Early in the pandemic, in April, the OMA selected BookJane as its technology solution partner to help address any labour shortages. Doctors could register through the app, and any hospital or health care facility could broadcast a service request to physicians across Ontario. That allowed matches in seconds.
In light of COVID-19, how can the health system and society as a whole function as safely as possible? Throughout the year the OMA was a critical voice in discussions, driving policy change by identifying key issues, conducting strategic government relations, and prompting the system to move.
The OMA also provided insight through major thought leadership, research and data analysis pieces. These dealt with diverse COVID-19-related topics, including PPE shortages, surgical times, mental health and addictions, physician payments and financial relief programs, drug shortages, and post-pandemic stress.
Activities included two white papers: the first released in May titled, Reopening Ontario to a “New Normal”: Five Public Health Pillars for a Safe Return; the other released in September titled, A Prescription for Ontario: Maintaining Vigilance as we Learn to Live with COVID-19.
Reopening Ontario to a “New Normal” was released when Ontario had managed to flatten the peak of its pandemic curve through a shutdown and strong physical distancing. However, without a vaccine or treatment, the risk of a surge remained. The white paper recommended a series of increased public health measures for the province to re-open safely:
At the time, OMA President Dr. Samantha Hill said: “The OMA and its members have an important role to play in using our expertise to provide thought leadership on issues that impact our health care system.”
The Prescription for Ontario: Maintaining Vigilance white paper provided recommendations on minimizing the spread of COVID-19, while tackling the ongoing backlog of medical services. It was based on lessons from the first wave of the pandemic and principles for going forward. Some takeaways:
Thought leadership isn’t just producing content, says Dr. Jim Wright, Chief, Economics, Policy & Research. It’s also being sought out by the government for advice. In managing the challenges of the pandemic, the OMA was a trusted voice at the table to proactively lead events to keep Ontarian’s safe, and to support members in meaningful ways.
From the start of the pandemic and throughout, the OMA weighed in as needed with timely counsel and insight. That touched on key areas like measures to increase social distancing, community spread and spread in long-term care settings, PPE needs, and funds for screening and assessment centres.
The OMA contributions have come at critical times. In July, for instance, as some areas of the province were moving toward Stage 3 of reopening, the OMA called on the government to rethink opening indoor bars. That was as outbreaks tied to indoor bars were occurring around the world.
And in November, the OMA suggested that the new framework for when regions can tighten and loosen pandemic restrictions is insufficient, at a time when the province is reporting record numbers of COVID-19 cases. The OMA recommended that the thresholds at which regions move from tier-to-tier should be much lower.
“Stakeholders are reaching out to us,” says Dr. Wright. The OMA’s input has helped Ontario adjust to COVID-19 and take steps to control it, and will continue to be invaluable throughout the course of the pandemic.
COVID-19 may be a physical disease, but its impacts on mental health can’t be overstated. The stress of the pandemic and the changes it has brought can be tough on anyone. That’s just as true for doctors as anyone, who have the added demands of being on the frontline. This is a race with no clear finish line.
The OMA’s Physician Health Program (PHP) – now in its 25th year of supporting members – isn’t a response to COVID-19, but is a valued resource to doctors dealing with stress, other mental health concerns and substance use. The PHP offers confidential support and services. What’s new this year is a wellness support line, funded by the CMA and piloted during COVID-19. If you have questions or need support, call 1-800-851-6606 or email php@oma.org.
In the members-only section of the website, the OMA has promoted PHP-led virtual groups, including daily drop-ins via Zoom – an online meeting place to exchange experiences, support and encouragement. The PHP expanded other support services during COVID-19, including facilitated groups for physician leaders and for women physicians (across Canada), and hosted a physician town hall on mental health and resilience.
The member section also included links or information around managing interpersonal relationships, or difficult physician-patient relationships. Other resources: online mindfulness sessions, a webinar on mental health in the context of COVID, and podcasts on burnout available on the physician health and wellness section.
For COVID-19-related or everyday stress and challenges, the OMA and the PHP is there for doctors.
COVID-19 represents an unprecedented challenge. Throughout, the OMA’s response has been a cross-functional collaboration led by our Economics, Policy & Research department. Together, COVID-19 efforts have supported and advocated for members, provided them with timely information, engaged with government, supported policy change, and communicated to the public.
Overall, the OMA’s response has been effective. What could the organization have done differently? For one, people working on the COVID-19 response experienced a sudden increase in workload. An even more successful response could have come from redeploying staff sooner, dividing staff into shifts, and engaging external support. Certain work might have benefited from more focus, a different approach or better timing – if only the OMA had had more time or resources.
The OMA also didn’t have a pandemic playbook before COVID-19, meaning that many process decisions were made on the fly. Developing an OMA public health crisis playbook would help immeasurably with future events. Still, Dr. Jim Wright praises the OMA’s ability to turn on a dime. Organizations talk about being nimble as a value, and that has manifested itself during COVID-19.
No planning will ever put you in a position where you can predict what will happen, states John Bozzo. The next crisis will be different than the current one. But you need the right processes, people and systems in place to be able to react, Bozzo says.
We are not at the end of the pandemic, but as we head into 2021, Dr. Wright is hopeful that we’re at the beginning of the end. Beyond the COVID-19-specific lessons, he says the experience of the year may trigger broader change. It can take a crisis, he says, to “galvanize people and have the population engage in what the health care system should look like.”
“What all crises do is shine a light on cracks in the system,” adds Bozzo. “One of the biggest is a lack of integration. There was also too much focus on acute care and not enough on long-term and community care. There’s an opportunity for the OMA and doctors to keep the light shining on those cracks, and hold the government to account to do something about it.”
Stuart Foxman is a Toronto-based writer.